Sort By...
THURSDAY, DECEMBER 18, 2025
“Unbearable: Five Women and the Perils of Pregnancy in America”: Author Conversation
Eighty percent of maternal deaths in the United States are considered preventable. So why do they keep happening?
On this episode of “Conversations on Health Care,” hosts Mark Masselli and Margaret Flinter are joined by award-winning journalist and New York Times bestselling author Irin Carmon for a thoughtful conversation about pregnancy, care, and what gets lost when she says systems stop listening.
Carmon’s new book, “Unbearable: Five Women and the Perils of Pregnancy in America,” draws on 15 years of reporting and the stories of five women navigating very different parts of the American maternal health system. Rather than a political argument, the discussion focuses on lived experience, reporting and what compassion and accountability can look like in maternal health care.
“Pregnancy can be a gift. But nothing can truly be considered a gift when it comes wrapped in coercion or paternalistic silence,” Carmon wrote.
Through these stories, Carmon explores why preventable tragedies still occur, even in places with advanced health care, and what she has learned by listening closely to patients, families and clinicians.
“We know what makes a difference. Listening when someone says something doesn’t feel right is as sophisticated as you need to get.”
The episode touches on maternal mortality, postpartum care, midwifery models and why improving outcomes starts with recognizing the humanity of the person who is pregnant.
THURSDAY, DECEMBER 4, 2025
Flu Cases Rising: “It’s Not Good,” Says Former CDC Dir. Dr. Tom Frieden
The doctor who once led the Centers for Disease Control and Prevention sees trouble ahead:
- There’s been a significant decrease in people taking the COVID and flu vaccines
- Europe is experiencing the worst flu season in years (an early indicator of problems in the U.S.)
- CDC data show that Influenza infections are growing or likely growing in 41 states
“It’s not good…what we have seen from Europe is a very early and very severe flu season, something that could mean more hospitalizations.”
Dr. Tom Frieden says confusing vaccine guidance, limited access and weakened public health systems are contributing to fewer shots in arms. He also shares insights from his new book, “The Formula for Better Health: How to Save Millions of Lives—Including Your Own.” He explains his “See, Believe, Create” formula for building a healthier future and his broader call for a public health system that listens to communities and makes vaccination easier. Dr. Frieden now leads Resolve to Save Lives, which works to close the gap between proven, life-saving solutions and the people who need them around the world.
MONDAY, NOVEMBER 24, 2025
Can You Have a ‘Healthy’ Thanksgiving? How the Food Industry Conspires Against Us
Leading nutritionist Marion Nestle, Ph.D., has a sobering message as we get ready for Thanksgiving: America’s food system delivers twice the calories we need while wasting 40%. “Thanksgiving provides five times the calories we need,” she points out. Her advice? “It is a week in which you just have to do the best you can.”
But once we've cleared the dishes after Thursday’s meal, Nestle offers practical advice for people trying to make healthy, budget-conscious choices as food prices continue to rise.
“If there is anything that is a superfood, it is a bean. If you want to save money on food, you have to cook.”
Nestle discusses the dramatic changes in our food system over the last 20 years, the growing influence of social media on what we buy and eat, and the rise of ultra-processed foods. She joins hosts Mark Masselli and Margaret Flinter to discuss her new book, “What to Eat Now,” an updated and expanded guide to navigating today’s food landscape.
Watch the full interview now.
Nestle’s earlier appearance on Conversations on Health Care is also available, where she discussed artificial food dyes, food industry marketing and the need for a food system that puts public health first. Click here to watch.
THURSDAY, NOVEMBER 20, 2025
How Dr. Sanjeev Arora Helped Improve Care for 200 Million Patients
People around the world are living longer and healthier lives because of an innovative idea that became a global force for change. On this episode of Conversations on Health Care, hosts Mark Masselli and Margaret Flinter welcome back Dr. Sanjeev Arora, founder of Project ECHO, an approach that has already improved care for more than 200 million patients worldwide.
Project ECHO was born from one question Dr. Arora asked himself more than 20 years ago: How do we make sure no patient is left behind because they cannot reach a specialist? What began as a hepatitis C initiative in New Mexico is now used for more than 70 complex conditions across over 200 countries and territories.
In this new interview, Dr. Arora reflects on what inspired him, what surprised him, and what he believes is possible next. He explains how primary care providers became force multipliers for specialty expertise, how Project ECHO expanded through COVID-19, and why community health centers continue to lead the way in democratizing knowledge.
“If we are willing to democratize our expertise and work together as interconnected providers, we can rapidly improve the U.S. health care system,” Dr. Arora said.
He also shares why the ECHO model boosts the resilience and joy of primary care teams, improves outcomes for underserved populations, and has transformed mental health care in India, where one psychiatrist may serve hundreds of thousands of patients.
“I know this work is making a difference in the community and in the world,” he said.
Listen to the full interview to hear Dr. Arora’s reflections on scaling impact, building health care communities, and the hope he carries for the next chapter of Project ECHO.
This episode also marks a meaningful return. Dr. Arora first appeared on Conversations on Health Care in 2011, shortly after Project ECHO was recognized as a disruptive innovation in global health. You can revisit that early conversation, here.
THURSDAY, NOVEMBER 13, 2025
“Cash for Moms and Babies”: How it Works & Why
What if health care for moms and babies came with a cash prescription for them?
In this Conversations on Health Care episode, hosts Mark Masselli and Margaret Flinter welcome back Dr. Mona Hanna, the Flint pediatrician whose research exposed the city’s water crisis and sparked a national reckoning on environmental justice.
Now, Dr. Hanna returns to share powerful results from Rx Kids, the nation’s first community-wide prenatal and infant cash prescription program. By providing unconditional financial support to pregnant women and new mothers, Rx Kids is improving maternal health, reducing infant deaths, and strengthening emotional well-being for families across Michigan.
“This is about investing in people’s humanity,” says Dr. Hanna. “When we provide the resources parents need to care for their babies, we create healthier families and stronger communities.”
Dr. Hanna explains how this simple but transformative idea, grounded in science, dignity, and love, has already reached more than 3,600 families in 11 Michigan communities and distributed $15 million in direct support. She also highlights how advocates can bring this program to their community.
Listen to the full interview.
You can also revisit Dr. Hanna’s earlier appearance on the program, where she discussed her pivotal role in uncovering the Flint lead water crisis and creating the Pediatric Public Health Initiative.
THURSDAY, NOVEMBER 6, 2025
Intimate Partner Violence: Health Care Providers’ Role
Intimate partner violence affects more women in the United States than breast cancer and diabetes combined. Health care providers can be a lifeline for survivors, yet many still struggle to know how to talk about it or where to begin.
In this Conversations on Health Care episode, hosts Mark Masselli and Margaret Flinter speak with Virginia Duplessis, associate director at Futures Without Violence and director of the National Health Resource Center on Domestic Violence. Duplessis shares how health care professionals can take practical, compassionate steps to identify, prevent and respond to domestic violence.
“Violence is not an inevitable part of the human experience. We all have a unique and important role to play,” says Duplessis.
Her work helps providers use trauma-informed care to start conversations with all patients about relationship safety and well-being. Through Health Partners on IPV + Exploitation, Futures Without Violence is building partnerships that make these conversations part of routine care.
Duplessis also highlights how prevention can begin early, from school-based programs like Coaching Boys into Men. Pregnancy and postpartum care also give providers more opportunities to build trust and spot warning signs.
“We want every patient to leave feeling supported, listened to and connected to information about what’s available in the community if they choose to seek help,” she says.
Click for the full interview now and explore the resources on domestic and sexual violence, child abuse and more.
THURSDAY, OCTOBER 30, 2025
Shutdown Threatens Food Benefits: Family Physicians Leader Urges Resolution
Food insecurity could soon worsen for millions of families and result in devastating health outcomes. American Academy of Family Physicians CEO Shawn Martin joins hosts Mark Masselli and Margaret Flinter to discuss how the government shutdown is putting the Supplemental Nutrition Assistance Program (SNAP) in jeopardy. Beginning on Saturday, Nov. 1, food assistance could end for up to 22 million recipients.
Martin and his 128,000 members are calling for bipartisan action to reopen the government and protect families from unnecessary harm.
“We must put the well-being of families first. Food insecurity is not a political issue—it’s a health issue, and every delay in action deepens the harm to our most vulnerable communities."
In this powerful conversation, Martin explores how hunger is showing up in exam rooms, the growing pressure on emergency food banks, and what policymakers must do to prevent a widening public health crisis.
Click for the full interview now.
THURSDAY, OCTOBER 23, 2025
New Research Bolsters Model for Preventing Infant Mortality
A recent report from the Centers for Disease Control and Prevention found that several Southeastern states continue to report the highest rates of late-pregnancy fetal death in the country. This is the kind of research that energizes Nurse-Family Partnership supporters to build on their mission to positively impact and transform the lives of first-time moms and their babies through a proven home visiting model.
The NFP model connects specially trained nurses with first-time mothers from early in pregnancy through the child’s second birthday.
Sharon Sprinkle, co-director of the partnership’s nursing practice, and Jenny Harper, its government affairs director, discuss with hosts Mark Masselli and Margaret Flinter the nonprofit’s founding, funding and how expectant moms can sign up.
Sprinkle says too often pregnant women say their concerns were “minimized or totally dismissed, when, in fact, if they were listened to, the outcome would have been better.
Originally broadcast June 5, 2024.
THURSDAY, OCTOBER 16, 2025
Preventing Veteran Suicides: Strategies & Tactics
Veterans Day, which is less than a month away, is a time to honor and reflect on those who’ve served. Yet statistics reveal a troubling reality: Veterans are dying by suicide at 1.5 times the rate of the general population. Suicide is now the second leading cause of death among veterans under 45.
Craig Bryan, clinical psychologist, Iraq War veteran, and author of “Rethinking Suicide: Why Prevention Fails and How We Can Do Better,” joined hosts Mark Masselli and Margaret Flinter to share critical research and real-world ideas for change.
Bryan challenges the long-held assumption that suicide prevention depends solely on mental health treatment. His work shows that more than half of veterans who die by suicide lack a prior mental health diagnosis, and that firearm safety, access to services, and new therapeutic models can make a real difference.
“Many of us were trained in firearm safety on the range. Now, we need to bring that same responsibility into our homes,” Bryan said.
This interview provides insights about how we engage with prevention and care for those who’ve served, including research on rapid escalation of suicidal crises. Bryan also highlights the life-saving potential of brief cognitive behavioral therapy (which has shown reductions in attempts of up to 60% in trials).
Originally broadcast June 18, 2024.
THURSDAY, OCTOBER 2, 2025
How Govt. Shutdown Affects Telemedicine
The federal government is shut down and the ripple effects are being felt. Legislation tied to the budget impasse also means Medicare telehealth flexibilities and the Acute Hospital Care at Home program expired early Wednesday morning.
“Most providers and hospital systems are taking calculated risks to continue care during this time, but long-term continuity depends on action by our telehealth champions in Washington to restore these flexibilities and ensure retroactive reimbursement,” says Kyle Zebley, senior vice president, public policy at the American Telemedicine Association.
Right before the shutdown he talked to hosts Mark Masselli and Margaret Flinter about the situation. “The stakes are enormous. We’re talking about millions of Americans…having access to the telehealth services. It’s a tremendous setback for our community.”
THURSDAY, SEPTEMBER 18, 2025
‘How Healing Works’ Author Dr. Wayne Jonas Explains His Approach
Dr. Wayne Jonas, who formerly led the National Institutes of Health Office of Alternative Medicine, now directs the Healing Works Foundation, which has a mission to “make whole person, integrative care regular and routine.”
“The data is very clear: most health does not come from going to your doctor and getting a diagnosis or treatment,” Jonas tells hosts Mark Masselli and Margaret Flinter. “The body is continually healing.”
Jonas shares the story of a man he calls “Joe,” a grandfather living with chronic back pain despite years of surgeries, injections and medications. The turning point came when Jonas asked Joe what mattered most.
“He said his back pain kept him from driving to see his grandkids and getting down on the floor to play with them,” Jonas explains.
Together with a physical therapist, Jonas reframed the goal: Joe wasn’t there for pain treatment; he was there to interact with his grandchildren. A regimen of stretching, hot tub treatments, and better sleep and stress management helped him do just that within weeks.
“He was engaged in his own self-care…his own self-healing capacity had been tapped,” Jonas says. “He saw the results and said, ‘What else have you got, Doc?’”
Jonas’s vision for whole-person care began during his Army service in Germany, where he saw physicians using acupuncture, herbal treatments and other integrative approaches.
Click to hear the full conversation.
THURSDAY, SEPTEMBER 4, 2025
RFK Jr.’s Vaccine Fight: ‘Threat to Good Public Health’
Supporters say Health and Human Services Secretary Robert F. Kennedy, Jr. is fulfilling his vision to be “pro-safety,” not anti-vaccine. His recent actions have included restricting COVID eligibility, dissolving expert panels, installing skeptical voices and defunding mRNA development.
Michael Osterholm, Ph.D., director of the Center for Infectious Disease Research and Policy, is pushing back and says, “I've never in my 50 years in public health experienced anything like this in terms of the threat to good public health.”
Osterholm and Mark Olshaker are the co-authors of a new book, “The Big One: How We Must Prepare for Future Deadly Pandemics.”
The effort to suspend development and availability of certain vaccines is “not based on science. It's not even based on a political philosophy. These are dangerous decisions that have been made and we will pay a big price for them as we are now in preparedness freefall,” Osterholm says.
“Conversations on Health Care” hosts Mark Masselli and Margaret Flinter ask him point-blank to respond to National Institutes of Health Director Dr. Jay Bhattacharya’s contention that they’re winding down mRNA vaccine development because the technology had “failed a crucial test: earning public trust.”
Osterholm responds that “distrust has been sown by the very people who are supposed to be promoting vaccines.” Olshaker says, “We've taken for granted how much vaccines have changed our lives.”
Osterholm adds, “There's still a substantial trust in public health. When you have a megaphone the size of one that the Secretary now has, it does start to basically drown out science … but I think we have to continue to remember that the science is on our side.”
WEDNESDAY, AUGUST 27, 2025
Mayo Clinic Doctor Leads The Patient Revolution: Insights & Tools to Improve Health Care
Dr. Victor Montori, a Mayo Clinic endocrinologist, internationally recognized researcher, and author of “Why We Revolt,” joins hosts Mark Masselli and Margaret Flinter to talk about what it really means to fix a health care system that he believes has lost its way.
Montori leads The Patient Revolution, a global movement aiming to make health care more elegant with “no waste or haste, focused on the biology and biography of each person, responsive to each patient’s problems, and minimally disruptive, of patients’ lives and loves.”
For example, the initiative offers tools and materials they’ve developed over the last 18 years to support patients and clinicians. The Plan Your Conversation cards help patients think through what they’d like to share and “practice” a conversation they’d like to have with the clinician. The cards can be used for any condition or issue and in any care setting.
“Revolution is not about branding. It’s about turning away from the processing of people, and toward care,” Montori explains. He yearns for a return to “careful and kind care for all,” and for health systems to re-center themselves on the relationships that make healing possible.
Click to hear the full conversation.
THURSDAY, AUGUST 21, 2025
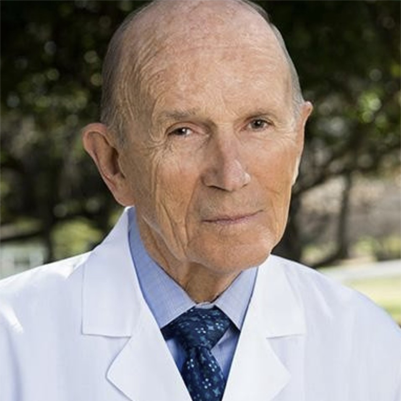
“Father of Aerobics” at 94: Dr. Cooper’s Unrelenting Health Advocacy
Dr. Kenneth Cooper’s FitnessGram is on the ropes. President Trump recently reestablished the Presidential Fitness Test; over 10 years ago, the government replaced the test with Dr. Cooper’s FitnessGram, “the first student fitness report card.”
Dr. Cooper has a cautious reaction. “Whether they’re going to be using exactly as the test [in the new process] is not really known. I am delighted to see that they realize the importance of childhood fitness.” To him, it just makes sense to measure fitness levels to help inform schools and families about how to help children get healthier. “Why don’t they test fitness like they test the mind? Data drives decisions.”
At 94, Dr. Cooper remains a passionate advocate for reshaping our national approach to health, particularly through the lens of prevention — a theme at the center of his new book, “Grow Healthier as You Grow Older.” He tells host Mark Masselli and Margaret Flinter, “We’ve got to stop and spend the money for the prevention of disease, rather than waiting for too much care, too late.”
Click to hear the full conversation.


.png)